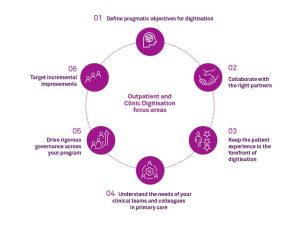
1. Define pragmatic objectives for digitisation
Why?
Defining your objectives help you, your stakeholders and program resources clarify what needs to be achieved. This helps with planning your digitisation project, as well as assessing the extent to which objectives have been met following implementation of the technology.
How?
Start by considering the areas for improvement and where digitisation can enable those improvements. Then consider how your program will contribute to your broader organisational strategy, and the patient journey, to determine the priority areas. For example, consider the following questions when developing program objectives:
- What are our aspirations for Outpatient and Clinic Service digitisation
- What problems is the digitisation program seeking to address?
- How can we improve the patient and the clinical teams’ experience?
- What are our funding requirements to help us achieve our objectives?
- Will our approach help us to meet state and territory guidelines for Outpatient and Clinic Services?
- What have others done and what lessons can we learn from them?
- How will we measure improvement?
2. Collaborate with the right partners
Why?
Finding a partner (or a group of partners) with expertise, solutions, tools and capabilities, can improve your chances of success.
How?
Assess potential partners alignment to your strategic goals, organisational footprint, partnership structure, and prior evidence-based Outpatient and Clinic Services transformation experience.
3. Keep the patient experience in the forefront of digitisation
Why?
Digitisation is not an end in itself – meeting patient needs, and expectations should be the focus, both in terms of improving patient experience and outcomes, and delivering patient-centric care.
How?
Engage with patients during the design process to understand their needs. You could do this through focus groups, design workshops, patient interviews or patient ‘tag alongs’. Once the solution has been implemented, support patient engagement components with an effective marketing campaign to increase adoption; and consider further engagement to understand the impact on the patient experience and the extent to which improvements have been achieved.
4. Understand the needs of your clinical teams and colleagues in primary care
Why?
You will be able to develop a solution that meets the needs of your clinical teams and key partners such as primary care, achieve buy-in, and increase adoption of the solution.
How?
Engage your clinical teams and key stakeholders such as GPs early in the project and provide ongoing opportunities for them to discuss how workflows and processes can be redesigned and effectively supported by technology.
5. Drive rigorous governance across your program
Why?
Having rigorous program governance increases the chance of program success. It enables clear decision making, effective communication between key stakeholders, and helps you control program outputs and outcomes.
How?
Develop a governance framework for your digitisation program at the outset – with clear roles, responsibilities, accountabilities, and information flows among program stakeholders. Consider how program governance will report into existing organisational governance structures.
6. Target incremental improvements
Why?
Targeting incremental improvements lets you manage the impact on the clinical and administration teams and changes to processes and workflows, to minimise disruption and manage change fatigue.
How?
Consider how you can digitise using an agile approach, that focuses on delivering improvements to your service and incremental process changes that’s supported by technology.
Understand what other digitisation initiatives are happening across your organisation and make sure your approach is aligned to the broader organisational approach and supported by effective change management.

 Visit
Visit